worst episode yet
This past Saturday, October 14th, started like any other Saturday… early rise, breakfast & off to sports.
We only recently left the hospital on Tuesday, October 3rd but Jack had recovered and been off oxygen since October 7th. He went to school Oct 9th through the 12th and seemed to be really enjoying himself and thriving. But Friday, the 13th, he woke up tired and we let him stay home.
Saturday the girls had early lax practices before their soccer games that afternoon. After those practices we were off to Jack’s soccer game. He started out fine, but half way through said that his legs hurt.
Fine, no problem - we took him home & got ready for Vivian’s game soon after.
At the start of the second half, after Jack had been unhappy for most of the game, he started begging to go home. Since I’ve been coaching Rylan all season, I really wanted to stay and watch the rest of Vivian’s game so Jason started packing up. Apparently Jack really wanted me to take him home and I simply said, “Jack you can come home with me but you have to wait for the end of the game.”
Before I even knew it, he was having a silent episode - crying without sound - and had started to stiffen & lose bladder control. I called for Jason to grab him & pick him up … we moved him away from the crowd and laid him down. He turned blue - passed out - and remained out for longer than usual. Folks around us who are medical professionals stepped in & assisted in CPR and called 911. Jack came back for a second, got upset & confused, and went into a second episode. This one was only 10 seconds or so - and he was alert before the paramedics arrived.
All who witnessed believed he was having a seizure - and due to the severity of the episode, and the fact that they continued to happen throughout the last week, we took the ambulance to Hopkins for further discussions.
The standard routine for us at the ED is - fight Jack for an IV, take blood, and put him on oxygen.
Monitor him … his oxygen always fluctuates between low 90s and high 80s *this is lower than the normal person.
And during episodes, his O2 drops into the 40s/50s - very bad.
The beeps & the monitoring of his oxygen have become a regular thing for us - and we always have to reeducate whatever nurse, resident, fellow, and attending that comes in over the course of several hours. Eventually, Jack’s given an anti-anxiety med and off to a fast MRI.
For a brain tumor, the first step is to make sure it hasn’t changed in size or has caused any bleeding or swelling. After that, we are back to the 11th (Pediatric Oncology) floor, where everybody knows our names (no, I’m not singing this to the Cheers theme song, unfortunately).
The nurses on this floor are amazing though - and I don’t have to tell them anything. They know Jack & they know us… but again, we retell the story to the residents and fellows.
This trip was different - this time - I refused to leave without answers….
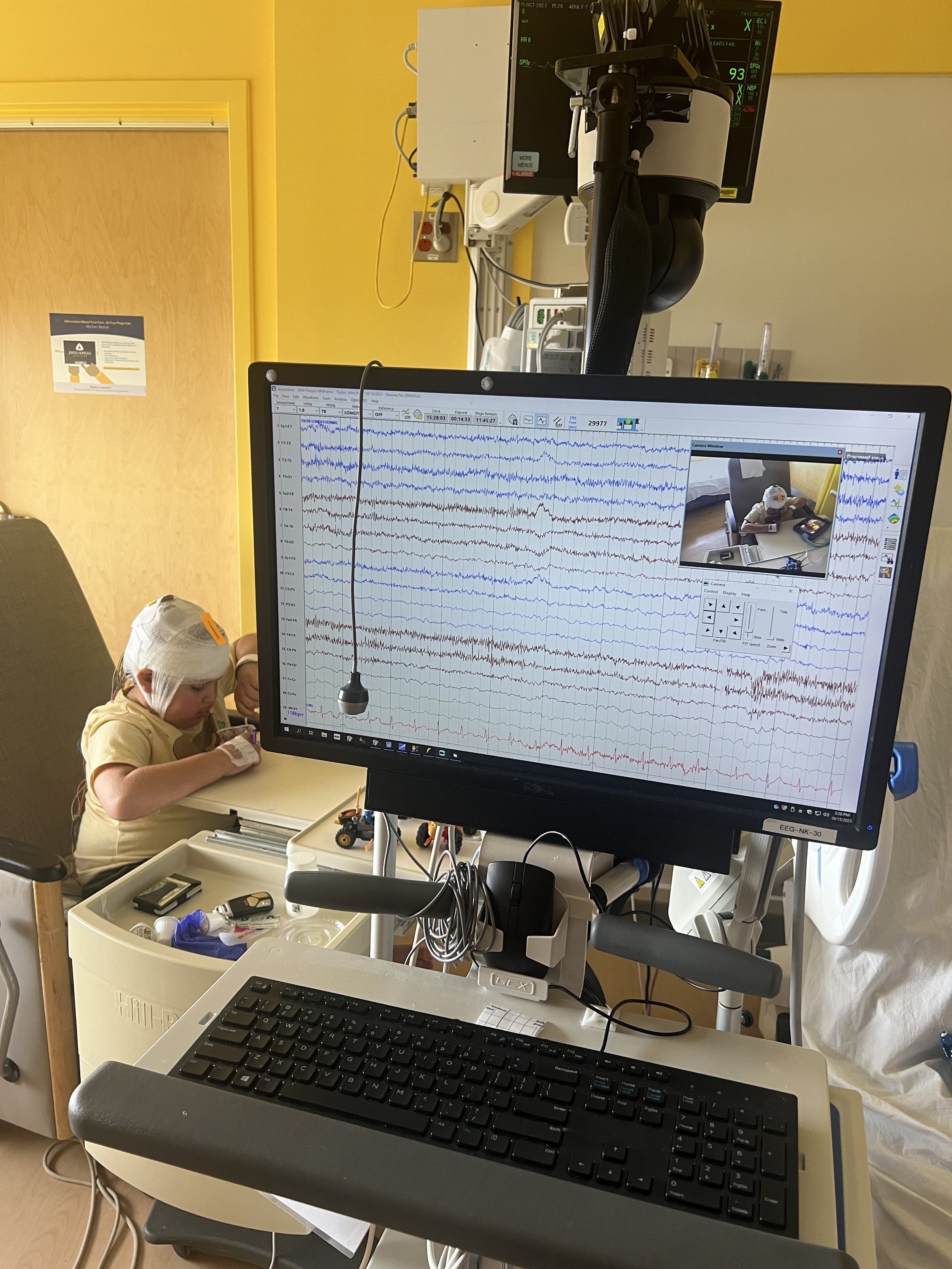
I demanded an EEG to rule out seizures. They’ve continued to say
“Jack’s tumor location doesn’t cause seizures.”
For 2.5 days, Jason and I forced an episode.
THIS WAS HELL.
He never had a full episode like the one on the soccer field - but he had a couple of mini episodes that never changed the EEG, ruling out epileptic seizures.
THEORY from their perspective is that Jack is having seizure like episodes from lack of oxygen…
IMPORTANT NOTE: ANTISEIZURE MEDICATION IN AN EMERGENCY COULD KILL JACK.
THIS WILL SLOW HIS BREATHING AND IS THE EXACT OPPOSITE OF WHAT WE NEED.
Please if you are ever in an emergency situation with us, please help us keep him safe by refusing this treatment.
Simultaneously, during these few days, our oncology team consulted with pulmonology - surprisingly enough, this was the first time during an admission.
A friend of mine had recently asked me, “have you talked to the pulmonologist Dr. Vanscoy, she is amazing and was the only one that could discover what issue my daughter was having?”
This was a few weeks ago & before this admission, I had reached out to consult with her but the clinic said I wasn’t allowed to switch providers. So then, I requested from Jack’s primary pulmonologist to have Dr. Vanscoy consult - but seemingly that never happened.
But on Day 2 of this stay, Dr. Vanscoy walked in…
As soon as she introduced herself, and I heard her name, I was relieved.
I thought she was there because I had requested her and she knew his story.
Shockingly enough - that was not the case. She had not known anything about Jack’s history.
She was told to come help us get Jack to tolerate a BiPap machine.
I was ten minutes into Jack’s story as I started to notice she looked puzzled.
This woman was so so kind and patient letting me talk and as I took a frustrated breath, she began to apologize and clarify why she was there. But what I had told her in that brief moment had her worried. She requested a day to read his history fully and come back to us tomorrow more prepared.
Respect, Dr. Vanscoy.
Absolute respect & a complete act of God that she walked in that day.
The first person we saw that next morning was Dr. Vanscoy.
She came in and had already scheduled a swallow study & chest CT for that afternoon.
She also ordered vest therapy & multiple masks for Jack to start tolerating BiPap.
Within less than 24 hours, this woman had completely changed our treatment plan and wanted to get to the bottom of Jack’s case. THANK GOD.
The CT scan told us that Jack’s lungs are in bad shape.
She said she was concerned that any more damage would get us to point of no return -
permanent lung damage -
The swallow study told us that Jack’s aspiration problem was still bad & some think worse.
NEXT STEPS -
G-Tube is their recommendation - and really the only one they have at this time.
To stop the damage to his lungs fast they want to bypass his throat & allow time for his lungs to fully heal. A G-tube will allow us to deliver his fluids & meds (any thin liquids) in a safe manner.
That, combined with multiple vest treatments & apnea sleeping machines, they are optimistic his lungs will heal and his oxygen baseline will improve.
To help with his obstructive apnea, if a G-tube is required then this is a good time to remove his adenoids and tonsils.
In the last several months, I had done a lot of research around vocal chord injections. While they are not sure if an injection will completely fix the swallow issue, they do not think it will hurt.
A lot in one surgery, but with Jack’s breathing issues & central apnea due to the brain tumor - less anesthesia events, the better.
SURGERY was today, October 20th, after being in the hospital all week waiting.
They began at 2:45pm & he came out of surgery - mad as hell around 5:30pm. He’s not fully awake yet but breathing on his own.
We are in the PICU all night for monitoring - hoping to hear his voice & normal self soon…
GOALS AND OUTLOOK
We are optimistic that this surgery will open his airway by removing the obstruction.
We are optimistic that the vocal chord injection will help with aspiration.
We are optimistic that the G-tube will only be temporary - to allow his lungs to heal.
We are optimistic that with all these improvements, his episodes will stop.